Unmitigated COVID is overwhelming hospital systems- globally.
From Canada to the UK to the US to Australia and beyond, media keeps framing the hospital crises as local and budget related. What about the elephant in the room?
There’s no doubt about it, public health systems everywhere are underfunded. Since neoliberalism grabbed the wheel of economic policy in the 1980s, there’s hardly a nation on Earth that hasn’t engaged in budget cuts to public services.
This austerity was the backdrop into which the COVID-19 bomb landed. Unsurprisingly, healthcare systems already in crisis struggled to handle the influx of patients. Unsurprisingly, hospitals with already strained capacity found COVID pushing them past the breaking point. Unsurprisingly, already understaffed hospitals struggled even more as workers went out sick short-term, long-term, and even died in the early waves.
Now, according to our world leaders, COVID is over. We’re back to normal! So normal, in fact, that reporters from every corner of the globe keep running the same article, week after week, country after country: gee, why are the ERs so overwhelmed?
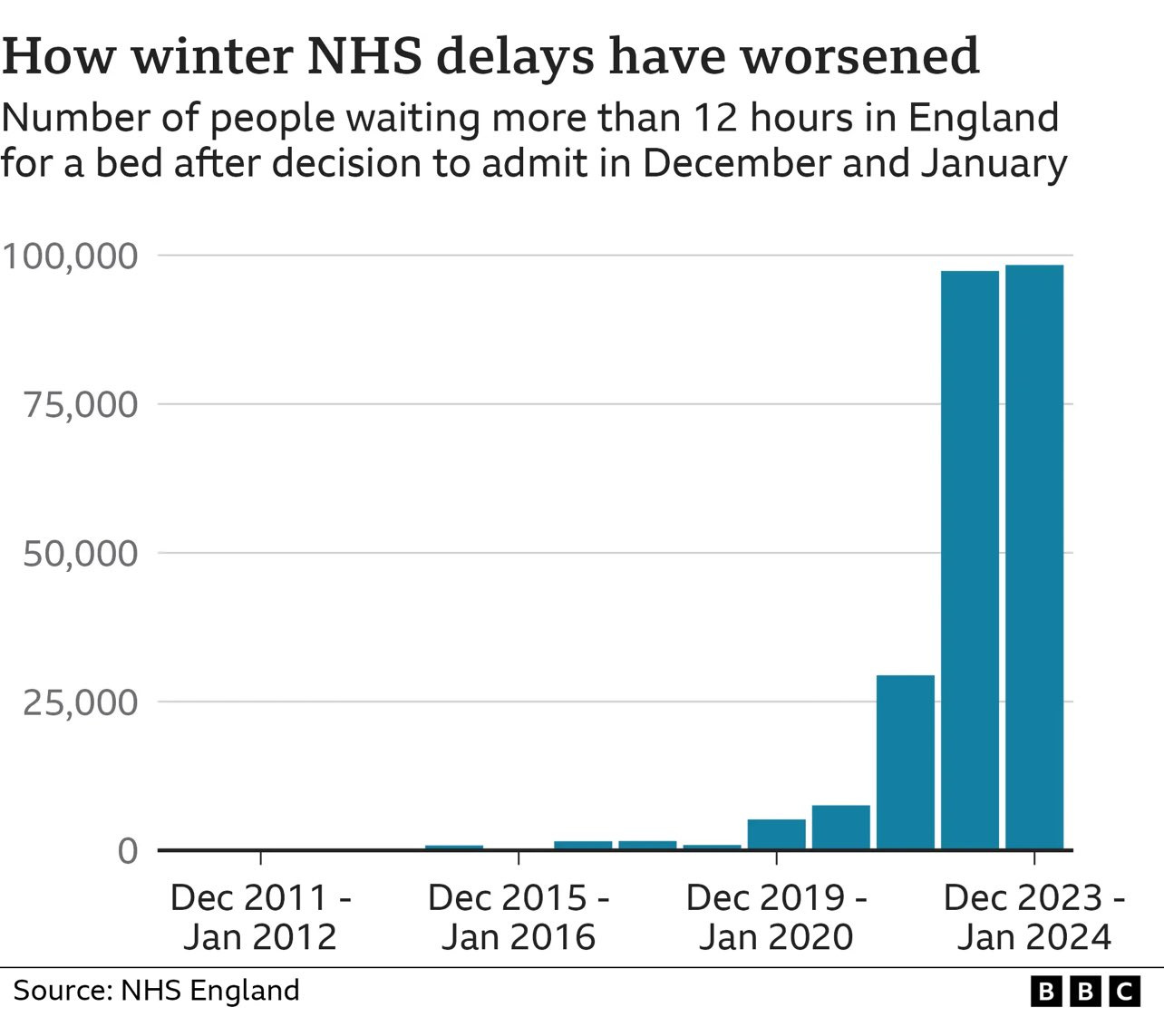
Sometimes a picture is worth a thousand words, so I’ll start with this graph from the BBC’s recent article, “12-hour A&E waits in winter ‘becoming normalised’”. Can you find 2020 on this graph?
The number of times this article, which again, published the above graph showing a precipitous increase in 12-hour-waits every year since 2020, mentions the word COVID, is zero.
This is, frankly, bizarre. It as if the author does not even remember COVID exists. Presenting a thorough accounting of the stresses on a collapsing healthcare system should of course include the recent introduction of a new, deadly virus with a tremendous health burden and high reinfection rate. Its exclusion is therefore an active choice, based either in denial or collusion. And it’s hardly an exceptional article; the incredible disappearing COVID phenomenon is everywhere.
The UK, in particular, seems to have a difficult time acknowledging that a strategy of “giving everyone a novel virus as often as possible” could possibly be in any way worsening their NHS crisis. This week, The Mirror published a piece titled, “NHS in crisis as patients stuck on trolleys pictured filling hospital corridors.” From the article:
In Liverpool's main university hospital trust - which includes Aintree and the Royal Liverpool Hospital - there were no patients waiting for 12 hours or more in January 2016. But by January 2024, this number had shot up to 1,427. The trust in Wirral, which includes Arrowe Park Hospital, saw a rise from no patients facing a 12-hour wait in January of 2016 to a whopping 915 in January of 2024. The St Helens and Knowsley Trust also saw a big jump from zero to 436 in the same months.
The article also, with zero irony, uses the term “post-COVID”.
It’s not that the NHS wasn’t in crisis prior to COVID-19; it’s simply that it is absurd to ignore the burden of COVID when talking about how that crisis has worsened. By every metric, on every graph, it’s quite clear where the COVID bombshell hit and it’s quite clear that health systems are unable to return to pre-COVID “normal”- despite our governments’ assurances otherwise.
The absurdity apparent in the UK reporting becomes even clearer when we look at the quite similar circumstances in emergency departments around the world.
Headlines from Canada:
In December, Ontario patients waited in ERs for an average of nearly 22 hours before being admitted to the hospital. (Macleans)
SickKids ICU reaches full capacity over the weekend as ER sees 'much longer than normal' wait times (CTV News Ontario)
Wait times for hospital admission from the ER are at a record high in Ontario. It’s a symptom of a system-wide crisis (Toronto Star)
Quebec's health-care crisis takes no vacation (Montreal Gazette)
Soaring ER wait times symptom of system-wide culture collapse (Winnipeg Free Press)
Growing concerns over ER capacity in N.B. and how it’s ‘busting at the seams’ (Global News)
190 Calgary doctors warn emergency rooms 'collapsing' in open letter (CBC News)
Emergency departments are in crisis now and for the foreseeable future (CMAJ)
Australia:
Record wait times in NSW hospital emergency departments, new figures show (The Guardian)
ED wait times and surgery waiting lists soar, new data shows (Australian Medical Association)
'People collapsing on the floor': Overcrowding and wait times at major Sydney hospital 'a disgrace' (9 News)
‘Crumbling system’: More sick Victorians endure 24-hour waits in emergency (The Age)
Patients abandoning care in Victoria's emergency rooms doubles as hospitals grapple with shortages (ABC)
US:
Emergency patients in Boston are waiting longer than ever for care (Boston Globe)
Uptick in patients at urgent cares, ERs causes long wait times in East Texas (KETK Tyler)
Hospitals ask patients with mild symptoms to avoid ER as respiratory illnesses surge (Indianapolis Star)
CT residents report days wait, adverse outcome, staff burnout due to emergency room overcrowding (Hartford Courant)
Patients Are Waiting Days for Care in Some California ERs (KQED)
Crisis in California? Emergency room wait times are skyrocketing as hospital space drops (Study Finds)
Minnesota emergency rooms get creative to meet ongoing patient overcrowding (StarTribune)
I’ve focused here on English-speaking nations because these are the headlines I’m constantly encountering, incredibly similar headlines from countries in very different parts of the world, all of them grasping desperately for some way to possibly improve these horrific ER wait times while either ignoring the existence of the ongoing pandemic, referring to it in the past tense, or lumping it in with “the flu”. (Lumping it in with the flu might not be so bad if the conversation then incorporated the adoption of airborne mitigations- they never do.)
But search any country, any city, anywhere, and these days you will find stories about overwhelmed ERs and record wait times. You will also find discussion of understaffing, budget cuts, and sometimes of unusual waves of illness. You will not find any calls to mitigate the novel virus imposing an unbearable burden on an already tenuous system.
There are myriad ways in which COVID is contributing to and worsening the hospital crises in all countries, extending far beyond the most obvious: acute illness. But let’s start with the ongoing, massive waves of acute infections. The lack of durable immunity to COVID is critical to understanding why a “let it rip” approach to this virus could never be sustainable. A recent preprint looking at immune evasion of the currently predominate variant, JN.1 found:
The overall effectiveness of previous infection in preventing reinfection with JN.1 was estimated at only 1.8% (95% CI: −9.3-12.6%). This effectiveness demonstrated a rapid decline over time since the previous infection, decreasing from 82.4% (95% CI: 40.9-94.7%) within 3 to less than 6 months after the previous infection to 50.9% (95% CI: −11.8-78.7%) in the subsequent 3 months, and further dropping to 18.3% (95% CI: −34.6-56.3%) in the subsequent 3 months. Ultimately, it reached a negligible level after one year. The findings show that the protection of natural infection against reinfection with JN.1 is strong only among those who were infected within the last 6 months, with variants such as XBB*. However, this protection wanes rapidly and is entirely lost one year after the previous infection. The findings support considerable immune evasion by JN.1.
In other words, if you get COVID now, you will get COVID again, likely within the next year (given our total lack of mitigation). The partial immunity provided by vaccination also fades rapidly, and COVID’s viral evolution continues to outpace vaccine manufacturers; this winter our boosters were formulated for the XBB variant, an ancestor of JN.1 that was no longer dominant by the time the boosters hit the market. Because of rapid viral evolution and rapidly waning immunity, we can never have herd immunity to this virus, not through infection, not through vaccination, not through a combination of both. Pursuing it as a public health strategy was a mistake.
Because of rapid viral evolution and rapidly waning immunity, we can never have herd immunity to this virus, not through infection, not through vaccination, not through a combination of both. Pursuing it as a public health strategy was a mistake.
This means that many, many more people are becoming acutely ill much, much more frequently than they were pre-pandemic. Studies have found that a typical adult only catches the flu about twice a decade. Even if COVID were a flu (it’s not), introducing a new virus with acute symptoms that reoccurs within months- not years- would represent a significant new burden on any health system. Acute illness also means more nurses and doctors are out sick in the short-term- especially since hospital systems refuse to implement airborne infection control and are thus continually sickening their own workers.
But acute illness is only one piece of the COVID puzzle. COVID also causes heart and vascular damage, leading to a higher burden of strokes, blood clots and heart attacks. An almost too-silly-to-be-believed headline in Bloomberg this week proclaimed, “A Spike in Heart Disease Deaths Since Covid Is Puzzling Scientists.” The very same outlet, Bloomberg, published “If You’ve Had Covid, Watch Out for Stroke Symptoms” in November 2022, “Covid-19 Tied to Higher Risk of Deadly Blood Clots in Large Study” in October 2022, and “Heart Damage Plagues Covid Survivors a Year After Infection, Study Shows” way back in October of 2021.
These types of patients are almost certain to end up in the ER and/or hospital. And long-term effects of COVID don’t stop at the heart; here’s a recent study from The Lancet showing increased long-term risk of lung diseases including asthma, COPD and lung cancer. The Financial Times piece “The growing evidence that Covid-19 is leaving people sicker” discusses increased risk of diabetes and cognitive damage. A recent study from Penn and Boston University found that the high excess deaths in the US since 2020 are driven by COVID.
COVID also can damage the immune system in various ways and is causing increases in the overall burden of other viruses, bacteria, and fungal infections. Although not every person who’s had COVID has damage or dysfunction of the immune system after every infection, frequently reinfecting an entire population with a virus that carries a significant risk of immune damage will inevitably result in a population that is significantly more vulnerable to infections.
Initial attempts to explain away the quite noticeable waves of illness with the anti-vaxxer “immunity debt” hypothesis went mainstream last year, but that “theory” appears to be losing steam as it becomes apparent that kids aren’t getting better. Emerging research continues to find increased vulnerability after COVID, for example, this study, which found that children with a previous COVID infection had a higher chance of a severe RSV infection. Long COVID patients were recently found to have dysregulation of the complement system, a part of the immune system that is a possible target for treatment.
As if the large excess illness and long-term health burdens of patients weren’t enough, we also have to consider the long-term illness burden of medical workers. Because hospitals aren’t implementing infection control, workers are becoming infected over and over again, and, shockingly enough, healthcare workers report a high rate of Long COVID. This means highly skilled, trained workers- already in short supply- are cutting hours and leaving healthcare long-term or even permanently.
A study in Brazil found a shocking 27% rate of Long COVID among infected healthcare workers. A British Medical Association poll published last summer found:
Doctors reported a wide range of symptoms, including fatigue, headaches, muscular pain, nerve damage, joint pain, ongoing respiratory problems and many more.
Around 60% of doctors told the BMA that post-acute Covid ill health has impacted on their ability to carry out day-to-day activities on a regular basis;
Almost one in five respondents (18%) reported that they were now unable to work due to their post-acute Covid ill-health;
Less than one in three (31%) doctors said they were working full-time, compared to more than half (57%) before the onset of their illness;
Nearly half (48%) said they have experienced some form of loss of earnings as a result of post-acute Covid;
54% of respondents acquired Covid-19 during the first wave of the pandemic in 2020, and 77% of these believed that they contracted Covid -19 in the workplace
These staggering findings were summed up in the outlet GP Online under the headline “Doctors with long COVID left 'penniless' as one in five unable to work”. The Royal College of Nursing (RCN) in the UK has been campaigning since the summer of 2022 to have Long COVID classified as an occupational disease.
And let’s not forget that widespread cognitive slowing isn’t conducive to efficiency and accuracy. A study published this month found “Attentional impairment and altered brain activity in healthcare workers after mild COVID-19”.
Yet in the many articles about HCW shortages and nursing shortages in particular, none of this is ever mentioned. Nor is it, strangely, by leftist organizers; in the UK, even activists who frequently comment on the NHS crisis seem allergic to the word COVID.
COVID is not a disease we can ignore out of existence; by now, that should be clear. We are sitting back and watching as the total capitulation to this virus worsens health outcomes both acutely and in the long-term. This anti-science COVID denial has led to high rates of hospital acquired infection and the death of patients. Continual reinfections are piling risk upon risk upon risk as previously healthy people ultimately develop heart, brain, lung, autoimmune, and other health problems. Increases in heart disease, strokes, and blood clots will continue to worsen as the public encounters its fourth, sixth, eighth reinfection.
What is the plan? 30 reinfections in 30 years?
The population-level damage of COVID reminds me of the population-level damage of climate change. Because the damage is so distributed, because it worsens gradually, and because it is so invisibilized by our media’s disjointed presentation, we continue to ignore what only our focused attention can remedy. Cities are facing record heat. Hospitals are facing record patient burdens. We must acknowledge and address these crises with a full accounting of how our individualism fuels them, and only collective action can address them.



Once again, you're right on target, Julia!!!